UrogynCREST Program
Funded by NICHD (R25-HD094667), the AUGS/DUKE Urogynecology Clinical Research Educational Scientist Training (UrogynCREST) Program is a 2-year online training program in pelvic floor disorders research and data science. Early-career faculty within approximately 7 years of fellowship who have a passion for research are invited to apply.
Participants will learn how to obtain, prepare, and analyze existing datasets to conduct their innovative research project. They will gain skills and confidence in programming, data manipulation, and directing their own statistical analyses. They will have opportunities to present their work at national conferences, and network and initiate collaborations with others in the field. By the end of Year 2, they are expected to publish their results in a peer-reviewed journal. Participants are expected to spend 20 hours per month on this program.
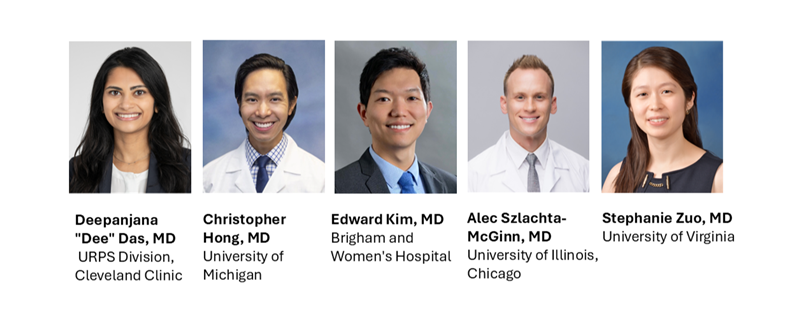
Cohort 4 (2024-2026)
The UrogynCREST program has four components:
- Year 1: Coursework
- Year 2: Mentor and Biostatistical Support, Data Access, Manuscript Submission
- Locating and Accessing Databases
- Dissemination and Networking

What Past UrogynCREST Participants Are Saying
Hear directly from previous cohorts about their experience working with our faculty and participating in UrogynCREST’s coursework!
I feel so fortunate to have had the opportunity to participate in the UrogynCREST Program. It was an excellent experience overall, and the opportunity to network with colleagues and leaders in urogynecology, access data, and complete additional didactic coursework on our own schedule was unlike anything else available for junior faculty interested in advancing their own early careers.
Melanie Meister, MD
The University of Kansas
The UrogynCREST fellowship has been a really incredible learning experience for me. The highlight was definitely being able to work with such dedicated mentors. [My mentors] were incredibly supportive, offering guidance without over-directing. They have been so responsive throughout, and I have learned so much as we worked through project development, statistical analysis, and manuscript edits. The icing on the cake is that this project will now be shared broadly in a very well-respected journal!
Lee Richter, MD
Georgetown University School of Medicine